Stories
Stories
Read the stories about our work, from those who do the work, and our upcoming programs, press releases, and project highlights.
View Page: Beyond the Last Mile: Fighting Malaria with Spot Checks and Integrity


Beyond the Last Mile: Fighting Malaria with Spot Checks and Integrity
View Page: The Affordable Medicines Program Is Helping Ukraine Achieve Health Equity Despite the War


The Affordable Medicines Program Is Helping Ukraine Achieve Health Equity Despite the War
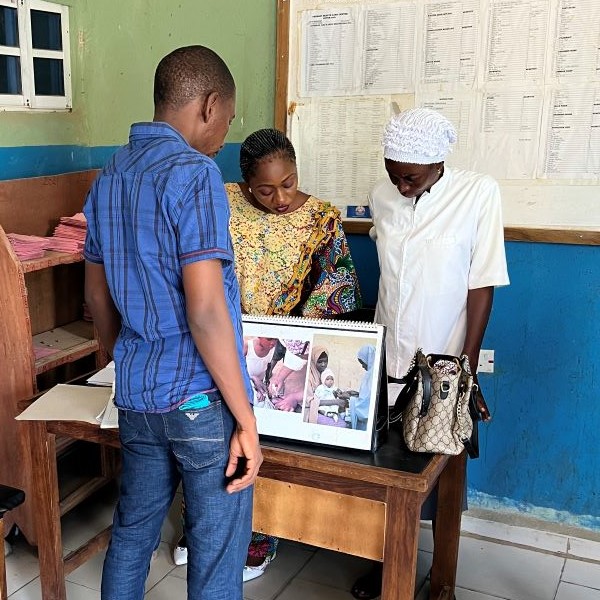
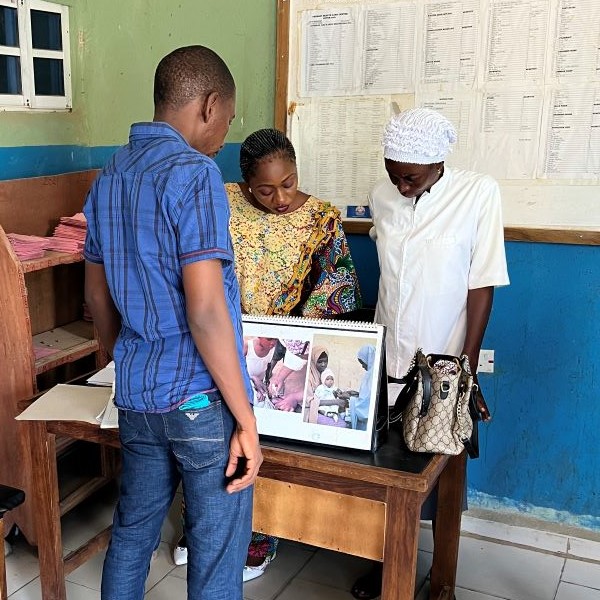
View Page: Using Treated Bed Nets to Fight Malaria in Nigeria’s Changing Climate Landscape


Using Treated Bed Nets to Fight Malaria in Nigeria’s Changing Climate Landscape
View Page: Management Sciences for Health, Beninese Government Continue Partnership with USAID to Strengthen Benin’s Health System
Management Sciences for Health, Beninese Government Continue Partnership with USAID to Strengthen Benin’s Health System
Arlington, VA—April 3, 2024—Management Sciences for Health (MSH) today announced it will continue its longstanding partnership with the Government of …
View Page: Management Sciences for Health Welcomes New Board Directors Magda Robalo and Ahmed Mushtaque Raza Chowdhury
Management Sciences for Health Welcomes New Board Directors Magda Robalo and Ahmed Mushtaque Raza Chowdhury
Arlington, VA—March 25, 2024—Management Sciences for Health (MSH) is pleased to welcome two new members to its Board of Directors: Magda Robalo and Ah…
View Page: Charting a Path to TB Elimination: Financing and Governance Strategies for High-Burden Countries


Charting a Path to TB Elimination: Financing and Governance Strategies for High-Burden Countries
View Page: Eliminating TB in Ethiopia: One Woman’s Journey Back to Health at Adare General Hospital


Eliminating TB in Ethiopia: One Woman’s Journey Back to Health at Adare General Hospital
View Page: Empowering Local Health Teams in Nigeria for Enhanced Governance in Malaria Programs
Empowering Local Health Teams in Nigeria for Enhanced Governance in Malaria Programs
View Page: Listening to the People’s Voice: MSH Convenes Discussion around New Survey Results


Listening to the People’s Voice: MSH Convenes Discussion around New Survey Results
View Page: Expert Voices: Dr. Alaine Nyaruhirira on Strong Laboratories Systems


Expert Voices: Dr. Alaine Nyaruhirira on Strong Laboratories Systems
View Page: MSH Joins with Mott MacDonald, ICF to Take on Stubborn Diagnostic Gap Problem


MSH Joins with Mott MacDonald, ICF to Take on Stubborn Diagnostic Gap Problem
View Page: Strengthening Lab Capacity to Save Lives: How MSH is Helping Ethiopia Eliminate TB

