Understanding the role of digital financial services for health: Lessons from case studies in Kenya and Rwanda
Understanding the role of digital financial services for health: Lessons from case studies in Kenya and Rwanda
By Management Sciences for Health, with contributions from USAID and Digital Square. It was originally published on Digital Square.
Even before the COVID-19 pandemic, 100 million people fell into extreme poverty annually because they couldn’t afford their health care, with women shouldering an unequal burden as primary caregivers. Meanwhile, countries around the globe are adopting digital tools designed to make it easier for patients to access and pay for health care, and to enable health providers and payers to improve management and operations.
Digital financial services (DFS) for health – which consist of banking, insurance, and payment services that can be accessed using digital technologies – are seen as an important lever toward the goal of achieving universal health coverage (UHC) in low- and middle-income countries.
More specifically, DFS for health include digital health insurance; health savings accounts; credit, transfers, remittances, and loans for health purposes; vouchers for health care; payments for health care/insurance by beneficiaries; and bulk purchases/payments across the health system, including payments to health workers.
To augment a systematic review conducted by USAID’s Local Health Systems Sustainability (LHSS) project, Management Sciences for Health (MSH) developed two programmatic case studies in Rwanda and Kenya to examine the innovative use of DFS for health to support UHC at scale:
- The Rwanda case study looks at the community‐based health insurance program managed centrally by the Rwanda Social Security Board that utilizes digital technologies for client management and mobile payments for clients to pay their insurance premiums.
- The Kenya case study focuses on multiple programs introduced by the PharmAccess Foundation including:
- The Innovative Partnership for Universal Sustainable Healthcare (i-PUSH) initiative that uses the M-TIBA mobile platform to connect low-income women of reproductive age and their families to health insurance and better-quality care.
- The Medical Credit Fund lending program that uses the CarePay technology platform and includes cash advance loans for health facilities and mobile asset financing loans for health providers to buy medical equipment.
With support from Digital Square at PATH, MSH developed the case study report through analysis of relevant data and interviews with dozens of beneficiaries, community health workers, mobile developers, health providers, and government officials. The research occurred during the COVID-19 pandemic, from June 2020 through August 2021, and incorporates views on the impact of the crisis. The case studies suggest that DFS for health can advance the UHC aim and strengthen health system performance, and they identify a variety of facilitators and barriers to implementing ‘DFS for health’ systems. Here’s more about what we learned:
WHAT WERE THE KEY DRIVERS FOR THE SHIFT TO DFS FOR HEALTH IN RWANDA AND KENYA?
Rwanda had been successful in covering a big slice of its population, now topping 80%, through its Community Based Health Insurance (CBHI) scheme, launched in 2005. However, after the CBHI scheme was centralized under the Rwanda Social Security Board (RSSB) in 2015, it became more difficult to manage paper-based enrollment and membership verification. To streamline this rising number of transactions, Rwanda developed 3MS (the Mutuelle Membership Management System) that same year to digitize membership management, and then added mobile payment options in 2018.

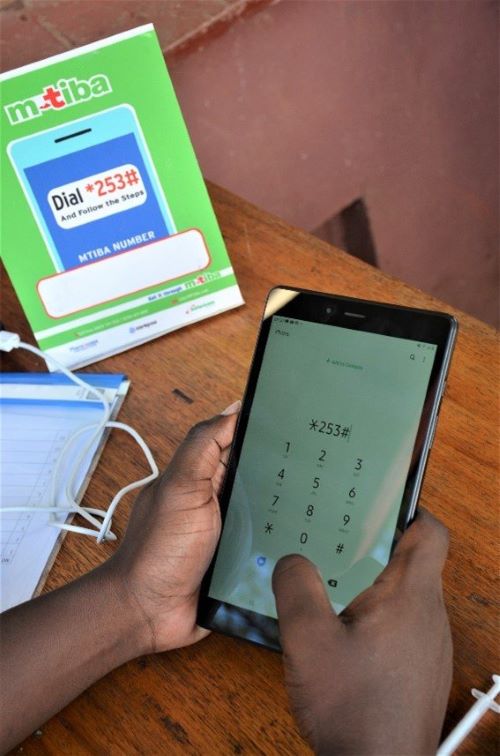
In Kenya, the social enterprise CarePay runs a digital health platform called M-TIBA which connects payers, health providers, and users in real-time–allowing for identification of users, and claims submission and handling among providers and payers.
Utilizing the M-TIBA mobile “health wallet”, the innovative Partnership for Sustainable Universal Health (i-PUSH) program was launched by PharmAccess to connect low-income women of reproductive age in Nairobi’s urban shantytowns and a remote western county to a digital savings plan to pay for enrollment in Kenya’s National Health Insurance Fund (NHIF). The program entitled them to free quality coverage for a year, with the expectation that they would begin contributing to the premium in the second year of participation.
Community health workers can use a combination of mobile apps built around the M-TIBA platform to enroll new members, educate their communities, and collect data for providers and health officials.
Thanks to i-PUSH and other similar initiatives, the M-TIBA platform used in Kenya has become a popular mobile payment system for the health care system (including government, retail, and private providers), connecting 4 million users and 1,200 providers. PharmAccess also introduced a complementary initiative to provide mobile loans for operational expenses and specialized equipment purchases to health service providers through the Medical Credit Fund.
WHAT WERE SOME COMMON TAKEAWAYS?
Both case studies reveal that moving away from a paper-based approach is boosting health insurance coverage, improving the quality and choices of health services, and helping households better prepare for health shocks.
Program participants also said they felt more engaged in managing their care by being able to pay premiums and check the status of their enrollment in real-time using their phone or via the internet.
Respondents in both case studies noted the importance of effective governance in establishing the enabling environment for DFS. For example, in Rwanda, the government’s ‘Zero Paper, Zero Trips’ vision for digital service delivery, support for increased internet connectivity, and easing of rules to encourage mobile payments helped pave the way for DFS innovations.
The case studies confirm that fully understanding and working with the existing service delivery infrastructure, whether it be mobile money agents or community health workers, is key to setting up systems that succeed. In Kenya, for example, the expertise from an established community of software developers contributed to the program’s success. “Nairobi has robust human resources for information and communications technology (ICT),” one participant noted. “The system was built for Kenyans by Kenyans who understand the context and the market and who are customer centric. It is easier for them to design and conceptualize the system to what the community needs.”
WHAT WAS THE IMPACT OF THE COVID-19 PANDEMIC?
The influence of the COVID-19 pandemic has been multilayered on both programs. In one sense, the fear of touching cash and engaging in in-person interactions early in the pandemic spurred interest in adoption of digital options that enabled enrollment in a health insurance scheme from the comfort of their homes, participants said.
But in some cases, enrollment in health However a big part of increasing enrollment in health insurance schemes is community focused, with community health workers “going door to door at the household level,” one participant said. So when the COVID-19 virus surged and lockdowns were declared, “work tended to stop.”

Similarly, staff promoting the Medical Credit Fund to health facility managers in Kenya were initially struggling to market their cash advance and medical assets loans “Because if movement is restricted then it means our foot soldiers cannot continue conducting the business of signing up new clients,” one participant said. Once they pivoted to marketing these services using virtual platforms, demand picked up again.
And although patients fearing the virus stayed away from hospitals during peak surges, with potential detrimental impact on individual health and provider finances, cash advances through the Medical Credit Fund allowed providers to receive upfront electronic payments to help cover costs during times when patient visits and revenue were low. Similarly, the Mobile Asset Financing program enabled health service providers to buy newly needed equipment, like ventilators, to help care for hospitalized COVID patients.
LOOKING FORWARD: LESSONS LEARNED THAT HELPED THESE PROGRAMS SUCCEED
Design programs based on the targeted population’s financial realities. In the i-PUSH program, for example, the expectation that very low-income women would be able to take on an increasing share of health insurance premiums after a year of subsidies proved overly optimistic, with only 12% contributing in the second year.
Use data collected through these DFS programs to identify and link needy beneficiaries to funding streams to help subsidize costs. This could include linking beneficiaries to relatives or government sponsored funding schemes.
Build on functioning community-based programs. Existing networks of community-based agents can provide education and build trust to use DFS, helping to bridge the digital divide.
Harness local infrastructure. Policymakers should work with the wide array of stakeholders to build on the existing digital landscape and infrastructure to forge ties across sectors in order to develop a shared vision for the country’s enterprise architecture and collaborate to implement a coordinated national digital health strategy.
Consider how to leverage transactional data generated by DFS for health for secondary uses. The wealth of data collected via DFS can be harnessed to better focus health programming, be more responsive to the needs of targeted populations, and help small business owners in the health sector establish credit histories in order to attract more investment.
Interoperability between DFS for health and other components of a country’s digital enterprise architecture is critically important. This can include mobile money payment gateways, health insurance systems, electronic health records, and national ID and income classification databases. Engage stakeholders that manage them early as efforts to build trust and negotiate data sharing agreements can be slow.
Finally, the study indicated that systems such as mobile loans, electronic payments, and mobile health wallets helped consumers and providers weather challenges associated with the COVID-19 pandemic. Health programs seeking to build resilience in the face of other health system shocks should consider these experiences and build DFS for health into their development initiatives.
Read the full report, “Digital Financial Services for Health: Programmatic Case Studies from Kenya and Rwanda.”