Data’s power and potential: Tanzania debuts electronic medical records to improve patient care and program planning
Data’s power and potential: Tanzania debuts electronic medical records to improve patient care and program planning
![[Speratus Macarius, a lab technician at Kigamboni Health Centre in Tanzania, checks a test order on the facility’s new electronic medical records system.]{Photo credit: Paul Bwathondi/MSH}](https://msh.org/wp-content/uploads/2019/04/tssp_715px.png)
With support from MSH, Tanzania is overhauling its digital health infrastructure, including introducing electronic medical records (EMRs) and a patient ID system, in hopes of dramatically improving its health services, especially for HIV/AIDS.
The country loses some 32,000 people each year to AIDS and an estimated 65,000 more are infected. Despite making good progress, it is stretching to meet global progress goals for HIV/AIDS programs. One major reason is that Tanzania’s data collection and health information systems are underdeveloped, fragmented and lack essential details, so they don’t deliver the quality information its health leaders need to monitor and plan patient and treatment outcomes.
The US President’s Emergency Plan for AIDS Relief (PEPFAR) supports Tanzania’s HIV program efforts, including funding the Technical Services Support Project (TSSP), which MSH leads. The project is helping Tanzania bring digital solutions to the health sector, including EMRs and a national patient registry, which will assign each person a unique health ID.
MSH is leading government ministries and NGO partners to coordinate roles and priorities and to figure out how to overcome the many and varied technical obstacles to merging data systems. It is a highly collaborative exercise that demands government commitment and ownership, which will pay off in a locally owned, sustainable solution.
TSSP Director Dr. Kenneth Lema said, “The Tanzanian government realizes the importance of accurate data to improve patient care, especially for HIV, and to make evidence-based decisions for its health system.”
A critical part of the project involved overseeing the development of the EMR system—including technical requirements, software development, training, implementation, and interoperability—and seamless integration with other electronic data systems, including the national hospital management information system (GoTHoMIS). The team has piloted the new system in six hospitals so far and plans to bring it to 16 facilities total by the end of 2019.
Early results are promising. Providers see more patients, are able to look at medical histories for better diagnoses, and can better adhere to established treatment standards and automate reporting. Facilities are better able to forecast medicines needs. Patients have shorter appointments and no longer need to tote their own paper medical records to them.
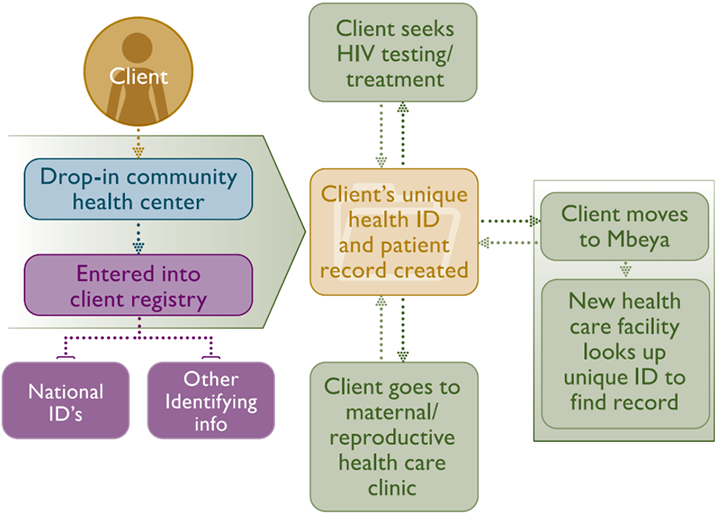
Next steps include developing a system for facilities to share health records and establishing a national health client registry system with patient IDs. This will provide a unique identifier for each patient that is linked to the national identification system and to family member records.
The Planned Health Client Registry in Tanzania
Information will flow from local health facilities to the central level, where it will enable advanced data analytics. With integrated records, public health institutions can better plan programs and track results. Human resources can be more appropriately allocated. Unified patient records will also contribute to better public health reporting and clinical research.
“These health data will be critical to improving HIV and other health services in Tanzania. We will have an overview of specific outcomes at health facilities, with which we can align investments and worker training,” said Paul Bwathondi, TSSP Deputy Project Director.
For more information, see the project brochure and brief.