Revision of the Group Perinatal Care Model Aims to Increase Participant Interaction & Reduce Travel Time
Revision of the Group Perinatal Care Model Aims to Increase Participant Interaction & Reduce Travel Time
This article was originally published by SCOPE.
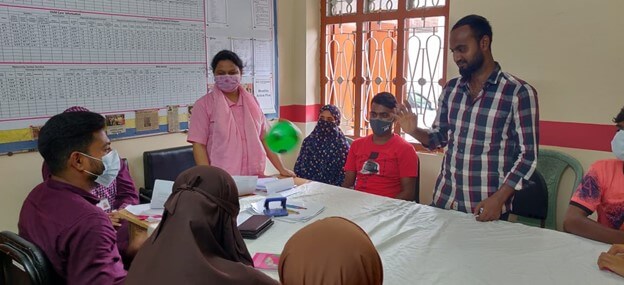
The Shustha Ma, Shustha Poribar, or Healthy Women, Healthy Families, seeks to improve the quality and use of maternal, newborn, and child health and family planning services and information among young women and their partners in the urban municipality of Tongi in Gazipur district, Bangladesh. The new service also aims to strengthen extrafamilial social support networks by enabling first-time pregnant women as well as recent mothers and fathers to share experiences and create bonds amongst each other, with facility providers and community health providers. This three-year project is led by Management Sciences for Health together with BRAC, Scope Impact, and The Population Council as innovation and implementation partners.
Conventionally, perinatal care has been provided on a one-to-one basis; however, in recent years group care models have emerged as a promising approach to deliver care more efficiently during and after pregnancy. The group model helps increase social support for pregnant women, building bonds between women and their care providers, as well as increasing the duration and quality of counselling information. This, by Scope Impact designed new model reflects women’s lived realities and provides an experience and content that meets their needs for emotional, social, and functional support through the perinatal journey. The process also involves husbands and other family members who often influence important care-seeking decisions during and after pregnancy.
As the model is tested in BRAC health centres, we have made adaptations and adjustments on an on-going basis based on real world implementation learnings. During the first reflection point, we conducted rapid exploratory research to understand the current challenges with the model across all stakeholders. We then utilised iterative, low-fidelity prototyping to improve upon the model or find new solutions. The key challenges that needed resolving included for example concerns around travel time to ANC/PNC/FP sessions and strengthening of retention between sessions. To reduce the travel time we identified community-based locations to be used for group sessions. To increase interaction between session participants and reduce the amount of time spent on didactic information sharing we adjusted the facilitation, increasing the number of activities that are participatory-first, encouraging group discussion before sharing information, and revising the way topics are talked about based on feedback gathered. To increase retention, we both crafted messaging to differentiate each group session during outreach, and included teasers at the end of each session about what would be covered next.
These changes are now being implemented across the BRAC health centres in Tongi with continuous monitoring and problem solving as needed. The project continues to test, iterate, and collect results through 2023.