Accelerating HIV Epidemic Control in Angola: a Sustainable Model for Comprehensive HIV Services
Accelerating HIV Epidemic Control in Angola: a Sustainable Model for Comprehensive HIV Services
“We want to provide excellent services to our patients; the same level of care they would receive in Paris, Thailand, or the United States of America.”
– Dr. Lombe Kilamba, an HIV Case Manager at Kilamba-Kiaxi Municipal Hospital
The Government of Angola is working to scale up early diagnosis and treatment of HIV. While the country’s HIV prevalence is lower than many of its neighbors, AIDS-related deaths increased by 33% between 2010 and 2018. The number of new infections is also on the rise, particularly among young women, and just 28% of adults and 13% of children living with HIV are receiving treatment.
To guide Angola’s response to HIV, MSH helped develop a sustainable continuum of care model for providing high-quality HIV and AIDS services and implemented it in collaboration with the Ministry of Health across seven health facilities in Luanda.
The model serves as a roadmap for the country’s efforts toward epidemic control: Between April 2017 and July 2019, nearly 173,000 people had been tested and more than 13,400 people living with HIV were diagnosed. Today, more than 17,000 Angolans are receiving HIV treatment in the seven project-supported health facilities, and 75 percent of patients on antiretroviral medication have achieved an undetectable viral load, making them much less likely to pass the virus to their sexual partners.
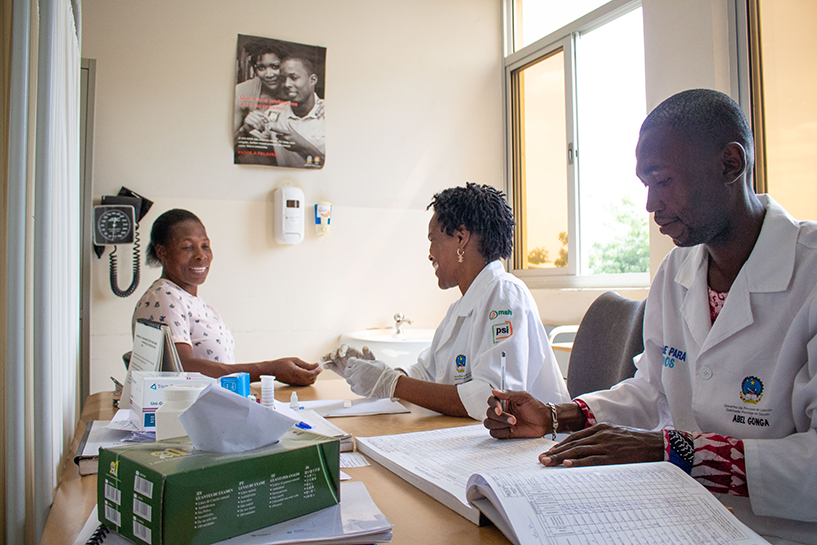
Grounded in a team-based case management approach delivered by patient assistant facilitators, community counselors, and case managers, this model considers a person’s journey from initial testing and HIV diagnosis through treatment initiation and sustained viral suppression.
Here’s how it works:
Patient assistant facilitators work with clinical teams to conduct active case finding, ensure adherence to treatment and retention in care through support services, and track those lost to follow up through phone calls. Many of these patient assistant facilitators are themselves living with HIV, acting as role models for sustained adherence and HIV management.
![[“Sharing my story helps people cope with a positive diagnosis and get the treatment they deserve and need to fulfill their lives,” says Manuela de Santos, a patient assistant facilitator. Ten years after her own HIV diagnosis, she acts as a role model for sustained adherence and HIV management.]](https://msh.org/wp-content/uploads/2019/11/img_2609_817px.png)
Once a positive case is identified, the patient assistant facilitator introduces the client to a community counselor. The community counselor is essential to deploying index case testing — a highly efficient and effective approach to identifying additional people living with HIV. She or he encourages the patient (index case) to identify sexual partners and family members who may have been exposed to HIV and then traces contacts and offers HIV testing, extending testing and counseling services into the community. When a contact tests positive, the community counselor escorts or directs the person to the health facility to be enrolled in treatment and overseen by a case manager.
![[To prevent inadvertent disclosure and stigma, community counselors also visit the homes of neighbors to share information about malaria, TB, and basic sanitation practices as well as HIV. Equipped with airtime to call contacts and rapid HIV test kits, community counselors are very effective in identifying new cases.]](https://msh.org/wp-content/uploads/2019/11/img_2668_817px.png)
Through index case testing, the project expanded testing and treatment services to the family and close contacts of nearly 5,000 newly identified HIV-positive patients and tested an additional 6,514 people, of whom 1,631 were identified as HIV positive. Case managers coordinate and oversee this team-based, patient-centered approach for all clients. They initiate and manage patients on antiretroviral treatment, conduct viral load tests, and ensure the provision of TB and family planning services.
Lastly, data clerks manage data collection, validation, and reporting.
“When we detect a new case, we immediately mobilize to start treatment that same day. We also try to understand the patient’s social situation. If they have a partner, we want to bring that partner in for testing. If they have children, we visit their home to test them too. This is what we do every day.”
— HIV Case Manager Dr. Lombe Kilamba.
The project initiated 8,479 newly diagnosed HIV-positive people on antiretroviral treatment — and over the course of three years, the percentage of HIV-positive individuals linked to HIV treatment increased from less than 40 percent to more than 70 percent.
![[More than 17,000 Angolans are receiving HIV treatment across seven project-supported health facilities and 75 percent of patients on antiretroviral medication have achieved an undetectable viral load.]](https://msh.org/wp-content/uploads/2019/11/mvi_3052.mov.00_01_55_26.still002_817px.png)
The tireless and unwavering dedication of these patient assistant facilitators, community counselors, case managers, nurses, and doctors is the foundation of an efficient and effective HIV program that provides all people living with HIV with respectful, comprehensive, patient-centered care. Locally led and delivered solutions like this are what it will take to end the HIV epidemic in Angola.
Related resources:
- Reaching the three 90s: Establishing a Sustainable Model for HIV Prevention, Care, and Treatment in Angola
- Reaching Families through Index Case Testing in Malawi
Led by Population Services International (PSI) and funded by the President’s Emergency Plan for AIDS Relief (PEPFAR) with support from the US Agency for International Development (USAID), Health For All was implemented in partnership with Management Sciences for Health and local partners Rede Mulher Angola, TechnoSaúde, Tropical Health, and the MENTOR Initiative. The project delivered a package of health interventions bringing malaria, HIV/AIDS, family planning services and reproductive health care in select municipalities and provinces throughout the country, reaching the poor and most vulnerable citizens of Angola.