Reaching Families through Index Case Testing in Malawi
Reaching Families through Index Case Testing in Malawi

An innovative testing strategy helps more people living with HIV learn their status
“Life can deceive you when you think you feel strong and healthy,” says Godfrey Justin, whose wife, Violet, tested positive for HIV during a routine antenatal visit. After sharing her status with Godfrey, Violet asked that he be tested as well. Godfrey agreed, learned he was also living with HIV and the couple started antiretroviral therapy (ART).
While traditional methods of HIV testing (such as provider referrals and client-initiated testing) successfully reach millions of people each year, only 75 percent of those living with HIV know their status. Reaching the 25 percent who don’t yet know their status — roughly 9 million individuals globally — will require more targeted approaches.
Reaching men and youth (ages 12 to 24) is critical to saving lives and preventing new infections. Data from high HIV-burden countries show that men access HIV testing and treatment services at lower rates than women and are therefore less likely to know their HIV status. This endangers both their own health and that of their sexual partners — often adolescents and young women.
“We reach many women through antenatal care visits, yet we are not able to reach men who are fending for their families … [or] youth who are mostly in school or who feel healthy and would not typically seek HIV testing services,” says MSH Project Director, Dr. Aziz Abdallah.
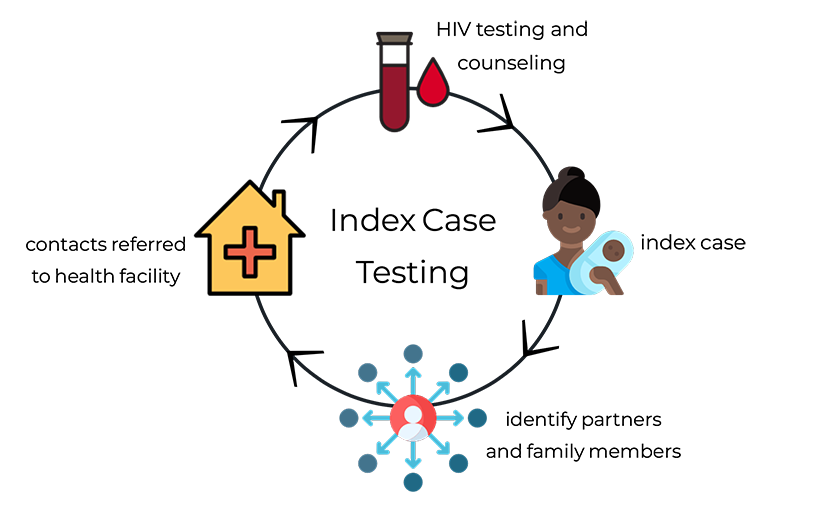
One strategy, pioneered in Malawi by MSH, is called index case testing. This methodology has been noted by UNAIDS as an emerging innovation for reaching more people living with HIV. Through this strategy, an individual who attends HIV testing services and learns that he or she is HIV positive becomes an index case. This index case client is asked to identify and refer others in his or her family or social network (such as a spouse, sexual partners, children, or siblings) to a health facility for HIV testing. Those who test positive are then asked to identify others at risk of infection and refer them for testing as well.
In Malawi, where the Justin family lives, the District Health System Strengthening and Quality Improvement for Service Delivery (DHSS) Project built upon this strategy by creating an enabling environment for index case testing to reach thousands of individuals.
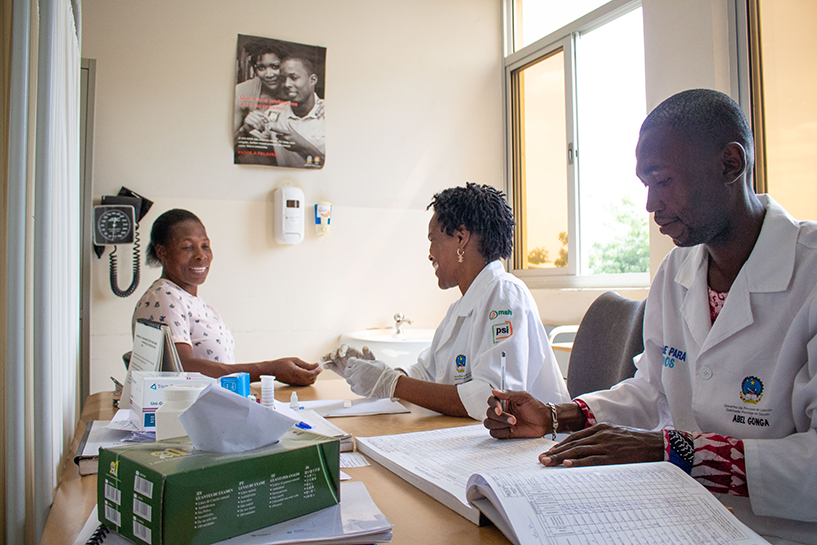
DHSS, funded by the US President’s Emergency Plan for Aids Relief (PEPFAR) through the US Centers for Disease Control and Prevention (CDC), supported Malawi’s Ministry of Health to recruit and train 190 HIV diagnostic assistants (HDA). These paraprofessional health workers are based in health facilities and dedicated entirely to HIV testing and counseling, freeing up doctors and nurses to focus on clinical management. This allows more clients to be tested and receive ART each day.
![[Gift Chitukula, an HIV diagnostic assistant (HDA) for Makhetha Health Center, talks with a client about the importance of partner and family testing.] {Photo Credit: Henry Nyaka/MSH.}](https://msh.org/wp-content/uploads/2018/08/hda_malawi._817px.png)
Family referral slips, simple paper forms designed by the Ministry of Health, are given to clients who test positive for HIV. With the HDA’s support, the client identifies sexual partners, children, and other family members who could also be at risk and completes a family referral slip for each person. The client then delivers the slip to each person, inviting her or him to receive testing services within two weeks. “The document helps give weight to the request to be tested,” said Jameson Chiwambo, an HDA at the health center where the Justin family received testing and counseling.
DHSS also introduced family testing days, special HIV testing clinics held on Saturdays at which newly tested clients are encouraged to bring in their loved ones for testing. By scheduling these open clinic days on the weekend, health facilities aim to better accommodate working individuals, in particular men and youth who are in school.
![[MSH’s supportive initiatives (such as HDAs dedicated to testing, family referral slips that positively reinforce the decision to be tested, lay counselors (expert clients) who encourage contacting partners, and family testing days that make testing more accessible) maximize the impact of the index case testing strategy.]](https://msh.org/wp-content/uploads/2018/08/dhss_index_case_testing_817px.png)
The decision to notify one’s partner or family member can be a very difficult one. Family testing days are organized in part by expert clients who mobilize their communities to attend and give motivational talks on the importance of partner and family testing. Expert clients are volunteers who have openly disclosed their HIV status in their communities and serve as role models for ART adherence. They are connected to their local health facility, provide psychosocial support and counseling for those who have been recently diagnosed, and encourage and support those who are notifying their partners and family.
![[ To create additional spaces specifically for HIV testing services, DHSS provided refurbished shipping containers to high-burden facilities, enabling 10 to 20 additional people to be tested each day.] {Photo credit: Moving Minds, Malawi.}](https://msh.org/wp-content/uploads/2018/08/img_1575_817px.png)
![[Left: After the introduction of index case testing by DHSS in June 2016, the number of people tested by project-supported facilities nearly doubled. Right: Of the HIV testing methods employed by DHSS, index case testing proved most effective in identifying new cases of HIV. *Provider-initiated testing and counseling (PITC)]](https://msh.org/wp-content/uploads/2018/08/dhss_report_graphics_817px.png)
In 2016, DHSS introduced index case testing to the 90 project-supported health facilities across six districts in Malawi. Within 13 months, over 5,500 individuals, or 22 percent, tested positive for HIV. This rate is much higher than the national average of 4 percent who are identified through traditional testing methods.
“Scaling up index case testing can help fast-track progress in Malawi as we move toward epidemic control,” says Rose Nyirenda, Director of the Department of HIV and AIDS in Malawi’s Ministry of Health.
Of those who tested positive, 98 percent initiated ART treatment. However, index case testing is not a stand-alone strategy, says Dr. Abdallah, who served as the Project Director for DHSS. “Index case testing complements traditional testing strategies by reaching into social networks and identifying more HIV-positive individuals,” he says.
As DHSS ended, Nicole Buono, Health Services Branch chief of the CDC in Malawi, promised, “We will continue to build on this initiative and the successes MSH has made in index testing …and we look forward to continue to learn and build on what was started by MSH.”
For Godfrey and Violet Justin, learning their HIV status and starting treatment has completely changed their family’s course. “We are living as a happy family and our health has been restored,” says Violet.
Learn about MSH’s approach to implementing index case testing in Malawi, Angola and Ethiopia: Reaching the First 90: A Webinar on Index Case Testing
![[A community volunteers provides free HIV tests at a local market in Eyokponung, Nigeria. Photo Credit: Gwenn Dubourthournieu/MSH]](https://msh.org/wp-content/uploads/2020/01/msh_eyokponung_market_09.05.2014_10_817.png)