Delivering Health for All through Joint Learning
Delivering Health for All through Joint Learning
![[Dr. Kamaliah leads participants in a discussion about measured performance of primary health care.]](https://msh.org/wp-content/uploads/2018/10/jln-hsr18-table1.817px.png)
This blog was originally published by the Joint Learning Network
We all know that working on UHC is a long and complicated endeavor,” said Modupe Ogundimu, the convener of the Joint Learning Network for Universal Health Coverage (JLN) Steering Group, “While it is possible for these goals to be brought together in a high-functioning system, it requires thorough knowledge and experience of what works, what does not, and how to apply the tools necessary for success.”
“That is where the JLN comes in.”
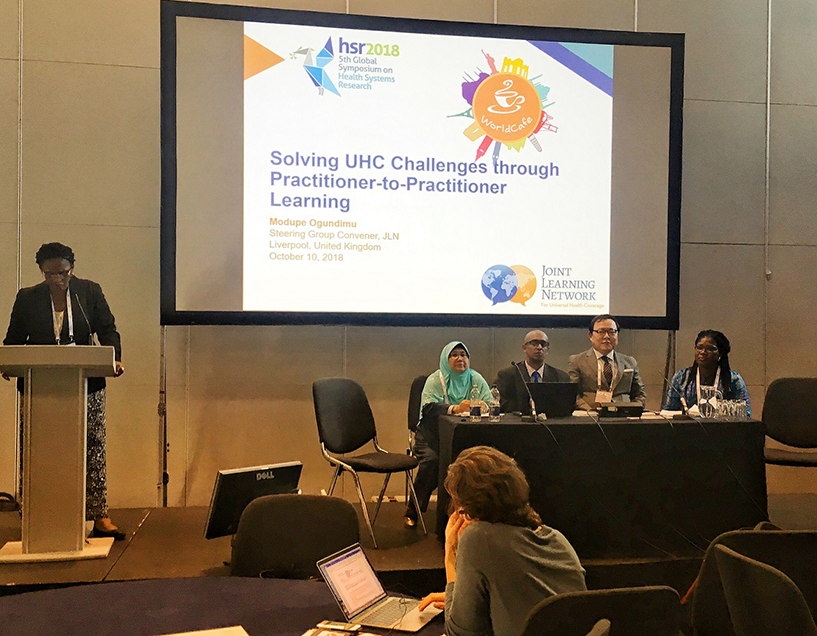
Modupe’s remarks kicked off an interactive 90 minute session at the Fifth Global Symposium on Health Systems Research organized by the JLN on October 10, 2018. Attendees at the session, Solving UHC Challenges through Practitioner-to-Practitioner Learning, met four JLN members from Kenya, Malaysia, Nigeria, and South Korea, for a mini-demonstration of the joint learning model:
- Dr. Omar Ahmed Omar Mohammed, Ministry of Health, Kenya
- Dr. Kamaliah Noh, Public Health and Community Medicine at Cyberjaya University College of Medical Sciences, Malaysia
- Dr. Nneka Orji, Senior Health Economist, Department of Health Planning Research and Statistics, Federal Ministry of Health, Nigeria
- John Ryu, Commissioner, International Cooperation Group, HIRA, South Korea
Joint Learning in Action
After a short introduction, the attendees self-selected into four small groups for facilitated discussions, led by our JLN members, about:
- Improving Primary Health Care through Measured Performance, led by Dr. Kamaliah Noh
- Balancing the Act of Designing a Health Benefits Policy, led by Dr. Omar Ahmed Omar Mohammed
- Making Quality and Cost Efficiency Gains in Health Care Services, led by John Ryu
- Domestic Resource Mobilization for Universal Health Coverage, led by Dr. Nneka Orji
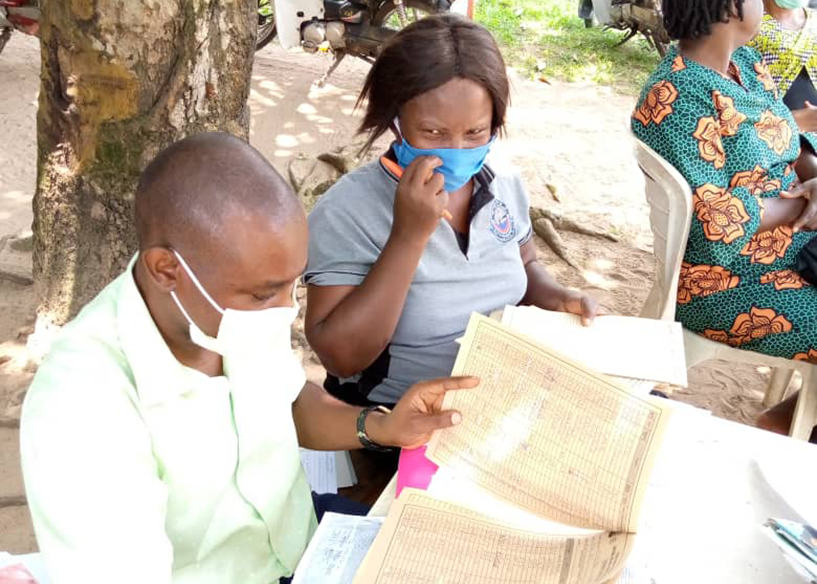
Discussing primary health care, Dr. Kamaliah emphasized the importance of measurement. Without a solid understanding of a primary health care system’s current performance, how can countries plan to make improvements? Setting a framework of what to measure, when to analyze, and how to translate data for decision-makers can help curate more actionable information.
![[Dr. Omar discusses the balancing act to bring interest groups together in the design of a health benefits policy.]](https://msh.org/wp-content/uploads/2018/10/jln-hsr18-table2.817px.png)
Dr. Omar shared a case study about Kenya’s experience designing a health benefits policy in a discussion that quickly focused on the stakeholder management challenges inherent in the creation of a health benefits policy to deliver universal health coverage. When a country commits to delivering health services for all, deciding which services are or are not included in a health benefits policy can be challenging, particularly when there is a broad set of stakeholders and interest groups each lobbying for their particular priorities.
![[John Ryu facilitates an engaging discussion about medical audit systems.]](https://msh.org/wp-content/uploads/2018/10/jln-hsr18-table3.817px.png)
With an understanding of measured performance and an idea of the services to include in their health benefits policy, how can countries drive improvements in the quality and cost efficiency of those health services? John’s breakout group discussed medical audit systems as one approach to do just that. These systems can provide helpful guidance and additional detail that practitioners can use to adapt.
![[Dr. Nneka shares her experience with domestic resource mobilization in Nigeria.]](https://msh.org/wp-content/uploads/2018/10/jln-hsr18-table4.817px.png)
But how do all of the services get paid for without imposing undue cost on people seeking care? Dr. Nneka used her experience in Nigeria to spark a discussion about mobilizing domestic resources. One reality that discussion participants wrestled with was the variety of options available for mobilizing resources–from reforming health financing mechanisms, advocating to donors and private-sector partners, identifying opportunities for cost-efficiencies, and more.
This abridged simulation of a facilitated joint learning session let participants experience for themselves what it feels like to participate in the JLN’s learning collaboratives, and further insight into how connecting peers from different countries, contexts, and experiences can promote learning and generate ideas to address shared challenges for universal health coverage.