Maternity Team Takes the Lead in Reducing Neonatal Mortality
Maternity Team Takes the Lead in Reducing Neonatal Mortality

Linda* arrived at Kibagabaga Hospital exhausted and desperate. Referred by a smaller health center, she had already been in labor for more than 24 hours. A midwife admitted Linda and put her on an IV. There, she waited for several hours until an obstetrician examined her. Realizing that the baby had an accelerated heartbeat, which is a sign of distress, the doctor ordered a Cesarean section (C-section). When the baby emerged, he was not responsive. Hospital staff worked to help him breathe and eventually, he let out a wail.
Asphyxia is an all-too-common challenge among newborns, and reducing it was recognized as a key priority as the Kibagabaga maternity team began MSH’s Leadership Development Program (LDP+), a participatory leadership development process that guides teams to face challenges and achieve results through action-based learning. Under the USAID-funded Rwanda Health Systems Strengthening (RHSS) Project, MSH collaborated with the Ministry of Health to launch the LDP+ course in Kibagabaga and Masaka hospitals to strengthen the leadership, management, and technical skills of health workers in their roles as health managers and providers.
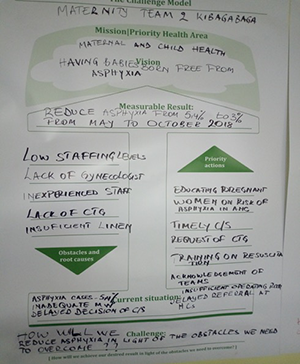
Kibagabaga Hospital’s maternity team created a challenge model to better understand the issue and to agree on a shared vision: That no babies born at the hospital would suffer asphyxia. The team set a target to reduce the rate of asphyxia from 5.4% to 3% between May and October 2018. Next, they developed a set of action steps to achieve their desired results, including reviewing the hospital’s protocols and discussing concrete actions for preventing asphyxia, reinforcing clear verbal communication between medical doctors and midwives during labor for timely decision making and between midwives and the surgical team to prepare for C-sections, closely monitoring a mother’s and baby’s vital signs during labor, auditing asphyxia cases, and acknowledging successful teams during handover session and in staff meetings.
With the support of hospital leadership and each team member’s commitment, the team reduced the neonatal asphyxia rate from 5.4% to 3.6%. Team members continue to carry out actions to meet the target asphyxia rate of 3% among newborns while sensitizing health providers and pregnant women on family planning and the standard four antenatal care (ANC) visits, timely reporting to the health facilities during onset of labor, and integrating asphyxia management into orientation training for new staff.
“Now the hospital staff take the lead and responsibility of managing and addressing challenges that come up in the respective services they deliver and motivate others where necessary.”
— Dr. Avite Mutaganzwa, Director General of Kibagabaga Hospital
Through the LDP+ training experience, the maternity team has learned that while clinical knowledge and skills are important to health worker performance, commitment to a shared goal and effective teamwork by clinical staff and hospital managers is paramount to reducing neonatal deaths and improving quality of care for mothers and babies.
*The person’s name in this story has been changed to protect privacy.