Moving Toward a New Model of Care for Afghan Mothers: The Critical Role of Midwives in Providing High-Quality Antenatal Care
Moving Toward a New Model of Care for Afghan Mothers: The Critical Role of Midwives in Providing High-Quality Antenatal Care
By Jennifer Gardella
Upholding quality of care is essential for achieving universal health coverage (UHC). A strong, responsive, and sustainable primary health care system—foundational for UHC—must ensure that quality, affordable, and person-centered health services are available and accessible to all, particularly vulnerable groups like women, children, and rural populations. This is especially imperative in fragile or emergency settings like Afghanistan, where quality can sometimes fall to the wayside in the interest of providing rapid, life-saving assistance.
While Afghanistan has made significant strides in establishing more widespread coverage of basic and essential health services over the last two decades, more work must be done to improve the quality of and increase access to quality care, particularly in maternal and newborn health. In Afghanistan, midwives play a vital role in providing primary health care for mothers and newborns in their communities, particularly in rural provinces. Afsana*, a midwife from Kandahar Province, reflects on the barriers that women face in accessing quality care in her country. “These communities are conservative,” she says. “Families are sometimes reluctant to let pregnant women visit the clinics for checkups, putting mothers’ and newborns’ lives in danger.”
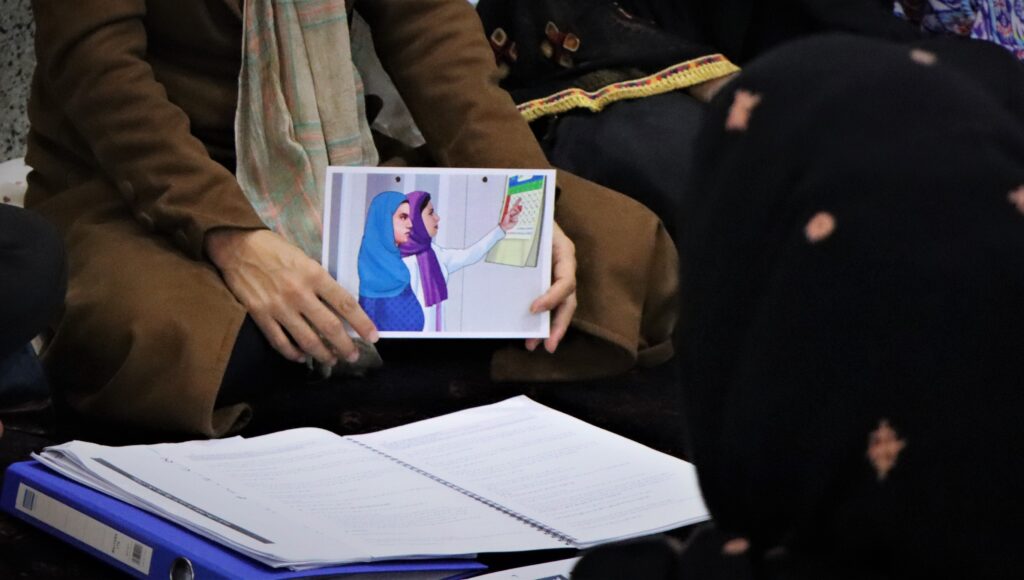
To better equip them with the knowledge and skills needed to provide high-quality care to pregnant women, the USAID-funded Assistance for Families and Indigent Afghans to Thrive (AFIAT) project is training midwives on an innovative approach that promotes a person-centered, culturally appropriate, group-based model of antenatal care (ANC). The model—based on the successes Management Sciences for Health (MSH) has achieved in implementing this model in other contexts—fundamentally shifts the power dynamics between patient and provider, allowing pregnant women to share their experiences in group settings, learn through peer-to-peer interaction, participate in social activities and games to build relationships, and receive individual routine checkups by the midwife alongside other expectant mothers.
This group antenatal care (GANC) model is one example of how MSH endeavors to put person-centered, high-quality primary health care at the forefront of our work. Since 2016, MSH has been piloting group-based ANC across several countries, adapting our interventions to meet the specific needs of each community. Building on the successes observed in Uganda, Kenya, and Guatemala and adapting the model to better suit a humanitarian context, MSH has most recently expanded this model to Afghanistan—and we are already seeing promising early findings.
Since September 2022, AFIAT has trained nearly 40 midwives from Kabul and Kandahar on the new GANC toolkit. Afsana participated in one of the first training sessions, which she described as more insightful and productive than any previous training she had received. “I have never participated in training of this caliber,” she says. “I learned a lot during the session, from the facilitators and from conversing with other attendees.”
During the training, Afsana learned alongside other midwives how to lead small cohorts of about 10 expectant mothers from their communities through monthly GANC sessions at their local health facilities. Over the course of the next six months, the midwives will lead sessions focused on supporting women as they navigate questions or challenges during their pregnancies; topics include birth plans, danger signs during pregnancy and labor, healthy birth spacing, infant and young child feeding methods, self-care during the postpartum period, and newborn care, including the importance of immunization and child growth monitoring. At each session, expectant mothers also learn techniques to conduct self-assessments at home and have an individual checkup with the midwife—which includes screening for antenatal depression, anemia, and malnutrition—to connect women to the right care at the right time during their pregnancies.
By taking this more participatory approach, midwives like Afsana generate acceptance among families, build trust in their communities, and offer expectant mothers a sense of community and sisterhood. At a time when Afghan women are increasingly isolated and disproportionately impacted by conflict and gender inequality, the GANC model of care represents a fundamental shift in how health services are traditionally provided for pregnant women in rural areas. This helps ensure a more dignified, empowered, and higher quality experience for patients and service providers alike, increasing the likelihood that pregnant women will attend these group sessions and protect their and their baby’s health.
Following the training, Afsana said that she looked forward to bringing the lessons learned during the training from the AFIAT team back to her community in Kandahar, where these new practices will help women and newborns receive the quality care that they need. “This new initiative will encourage women to visit their local health centers with confidence for routine checkups during pregnancy and after they give birth,” she says.
Since launching the GANC cohorts in October 2022, AFIAT has enrolled approximately 120 expectant mothers in 12 GANC cohorts across 6 primary health care facilities in Kandahar and Kabul. Following the second round of GANC sessions of the first cohorts—which boasted a 100% retention rate—all 60 of the participating mothers reported having plans to deliver their pregnancies at their local health facility, while 63% of the women could correctly recall the danger signs during pregnancy. Some first-time mothers attended the sessions with their mothers-in-law who were also interested in learning about these topics, indicating that the approach is already helping to build acceptance among some families. Due to the knowledge gained during the sessions, one participant recognized that she was experiencing signs of early labor at 28 weeks; as a result, she sought immediate care with the midwife from her group, who helped her access quality care so she could give birth safely and deliver a healthy baby. Additionally, after attending their individual ANC checkups, two women were referred to psychosocial counseling to receive support for antenatal depression.
The GANC approach—which will be expanded to all 14 AFIAT-supported provinces—is a notable recent example of MSH’s decades-long commitment to pursuing innovation and adapting interventions to achieve health for all in some of the world’s most challenging contexts. Through AFIAT, MSH continues its work alongside local partners in Afghanistan help foster the growth of a health system that prioritizes quality of care and is responsive to the needs of its most vulnerable people.
*Name changed for privacy.