Addressing the Global Crisis of Antimicrobial Resistance through Evidence and Action
Addressing the Global Crisis of Antimicrobial Resistance through Evidence and Action

The escalating threat of antimicrobial resistance (AMR) poses a grave challenge to global health. Overuse and misuse of antibiotics, antivirals, and other antimicrobial agents have fueled the emergence of pathogens that don’t respond to available treatments, making once manageable infections potentially lethal. AMR compromises the treatment of disease and poses a risk to global health security. Urgent and coordinated efforts on a global scale are imperative to address this crisis. The peer-reviewed journal articles below highlight MSH’s recent contributions to the evidence base of what works in the fight against AMR.

WHO Global Research Priorities for Antimicrobial Resistance in Human Health
Significant knowledge gaps are hindering effective responses to antimicrobial resistance (AMR), particularly in low- and middle-income countries, despite an increase in focus on the subject in recent years. The World Health Organization (WHO) has identified 40 priorities in its AMR agenda for 2030 to encourage research and investment that improve understanding of AMR dynamics and support policy translation. The authors and collaborators on the project, including MSH’s Mohan P. Joshi, present the WHO’s first comprehensive effort to prioritize research on drug-resistant bacteria and fungi, using a rigorous and validated methodology.
Supply-Chain Factors and Antimicrobial Stewardship
Weak supply chains in low- and middle-income countries frequently result in shortages of essential medicines, including antimicrobials, leading to the inappropriate use of alternatives and escalating antimicrobial resistance. The authors, including MSH’s Ndinda Kusu, examined the impact of health supply chains on antimicrobial use in Kenya, Malawi, Nigeria, Sierra Leone, Uganda, Tanzania, and Zambia to develop strategies for improving supply-chain effectiveness in supporting antimicrobial stewardship efforts.


A One Health Approach to Fight Antimicrobial Resistance in Uganda: Implementation Experience, Results, and Lessons Learned
Uganda has been working to improve its health security capacity in line with WHO benchmarks as it remains vulnerable to frequent disease outbreaks, including Ebola, yellow fever, COVID-19, and cholera. Antimicrobial resistance also remains a significant challenge. This paper—co-authored by MSH’s Reuben Kiggundu, J.P. Waswa, Niranjan Konduri, Hassan Kasujja, Marion Murungi, Eric Lugada, Cecilia Muiva, Esther Were, Dinah Tjipura, Kate Kikule, Emmanuel Nfor, and Mohan P. Joshi—details the technical assistance provided to Uganda by the USAID MTaPS Program using a One Health approach.
Infection Prevention and Control Compliance During COVID-19 Pandemic Era: Assessment of 26 Regional Referral Hospitals in Tanzania
Infection prevention and control (IPC) implementation at referral hospitals in Tanzania remains insufficient, despite ongoing efforts to build IPC capacity. This inadequacy continues to undermine the quality of health services, as poor IPC practices contribute to health care-associated infections and exacerbate antimicrobial resistance. This study aimed to assess the implementation of IPC practices across functional units in 26 regional referral hospitals in 2021.

A Bottom-Up, One Health Approach to Assessing Progress in the Implementation of a National Action Plan for Combating Antimicrobial Resistance: A Case Study from Uganda
Relying solely on desk reviews and national-level stakeholder engagement can overestimate a country’s health security and AMR capacity. Engaging frontline implementers, such as health care workers, farmers, and local governments, provides a more accurate assessment. This study—co-authored by MSH’s J.P. Waswa, Hassan Kasujja, Fozo Alombah, Mohan P. Joshi, and Niranjan Konduri—used a bottom-up approach to evaluate Uganda’s National Action Plan on AMR (NAP-AMR), thereby ensuring that subnational stakeholders were involved. The review exposed the poor engagement of these stakeholders and identified national-level issues, such as gaps in One Health policy, insufficient funding, and weak coordination, leading to inadequate NAP-AMR implementation. Addressing these issues requires establishing a One Health policy, securing sustainable funding, and legislating a dedicated policy to integrate the National One Health Platform into government structures.
Integration of IPC/WASH Critical Conditions into Quality of Care and Quality Improvement Tools and Processes: Bangladesh Case Study
Unsafe patient care in hospitals, particularly in low- and middle-income countries, often stems from inadequate infection prevention and control practices, insufficient support for water, sanitation, and hygiene (WASH), and poor waste management. This study, co-authored by MSH’s Tamara Hafner and Mohan P. Joshi, explored the intersection of IPC, WASH, and global efforts to improve health care quality, with a focus on maternal and newborn care in Bangladesh health facilities. Strategizing with stakeholders working on initiatives such as universal health coverage and patient safety to integrate IPC/WASH into quality improvement documents is a mutually reinforcing approach.

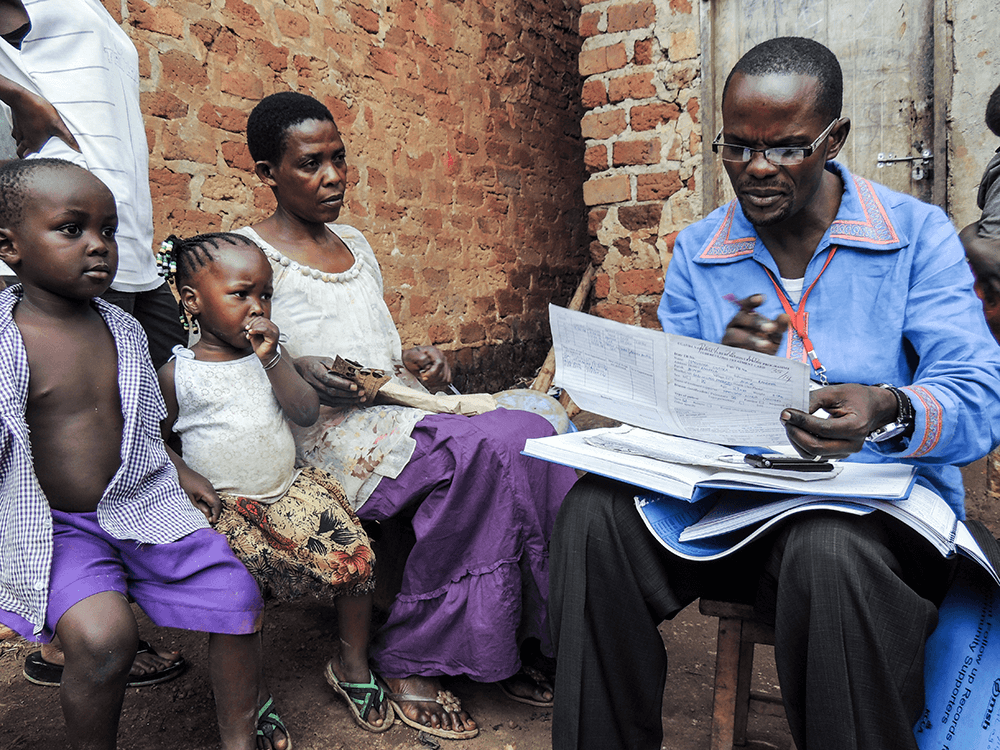
![[A client is counseled by a health worker on adherence to her medicine; Uganda.] {Photo credit: MSH staff.}](https://msh.org/wp-content/uploads/2014/03/img_1955_web.jpg)
Development and Evaluation of a Continuous Quality Improvement Programme for Antimicrobial Stewardship in Six Hospitals in Uganda
With support from MTaPS, six Ugandan hospitals conducted antimicrobial stewardship interventions targeting prevalent conditions linked to inappropriate antibiotic use, including urinary tract infections, upper respiratory tract infections, and surgical antibiotic prophylaxis. This article, which outlines the impact of these interventions, was co-authored by MSH’s Reuben Kiggundu, JP Waswa, Hassan Kasujja, Marion Murungi, Mohan P. Joshi, and Niranjan Konduri.
Moving from Assessments to Implementation: Promising Practices for Strengthening Multisectoral Antimicrobial Resistance Containment Capacity
This paper outlines four promising practices for enhancing national AMR containment capacity in 13 countries and was co-authored by MSH’s Mohan P. Joshi, Fozo Alombah, Niranjan Konduri, Antoine Ndiaye, Ndinda Kusu, Reuben Kiggundu, Edgar Lusaya, Robert Tuala Tuala, Martha Embrey, Tamara Hafner, Ousmane Traore, Mame Mbaye, Babatunde Akinola, Alphonse Acho, Yacouba Hema, Workineh Getahun, Md Abu Sayem, and Emmanuel Nfor.


What Is the Appropriate Antimicrobial Use Surveillance Tool at the Health Facility Level for Uganda and Other Low- and Middle-Income Countries?
Effective antimicrobial use (AMU) surveillance systems are crucial for guiding stewardship interventions, yet Uganda and other low- and middle-income countries face challenges in establishing them. This study—co-authored by MSH’s JP Waswa, Reuben Kiggundu, Niranjan Konduri, Hassan Kasujja, and Mohan P. Joshi—explores solutions.
National Consumption of Antimicrobials in Tanzania: 2017–2019
This was the first study from the sub-Saharan Africa region to offer a comprehensive analysis of antimicrobial consumption trends in Tanzania, and it provides recommendations for future research and interventions to combat AMR in the country. MSH co-authors include Edgar Lusaya and Niranjan Konduri.


Optimizing Prophylactic Antibiotic Use among Surgery Patients in Ethiopian Hospitals
In support of Ethiopia’s One Health approach to address AMR, MTaPS evaluated a quality improvement intervention in five Ethiopian hospitals from January to May 2023 focused on optimizing AMU for surgical prophylaxis. MSH co-authors include Getachew Alemkere, Hailu Tadeg, Workineh Getahun, Mohan P. Joshi, and Niranjan Konduri.
Gaps in Data Collection for Sex and Gender Must Be Addressed in Point Prevalence Surveys on Antibiotic Use
This article provides valuable insights into the importance of collecting sex-disaggregated and gender-specific data in antibiotic use surveys. Co-authored by MSH’s Niranjan Konduri, Nkatha Gitonga, Reuben Kiggundu, and Mame Mbaye, the article underscores the challenges associated with gathering such data while highlighting its potential to combat AMR and advance health equity.

Addressing Gaps in AMR Awareness in the Public: An Evidence-Based Policy Brief to Guide School Curriculum Review in Uganda
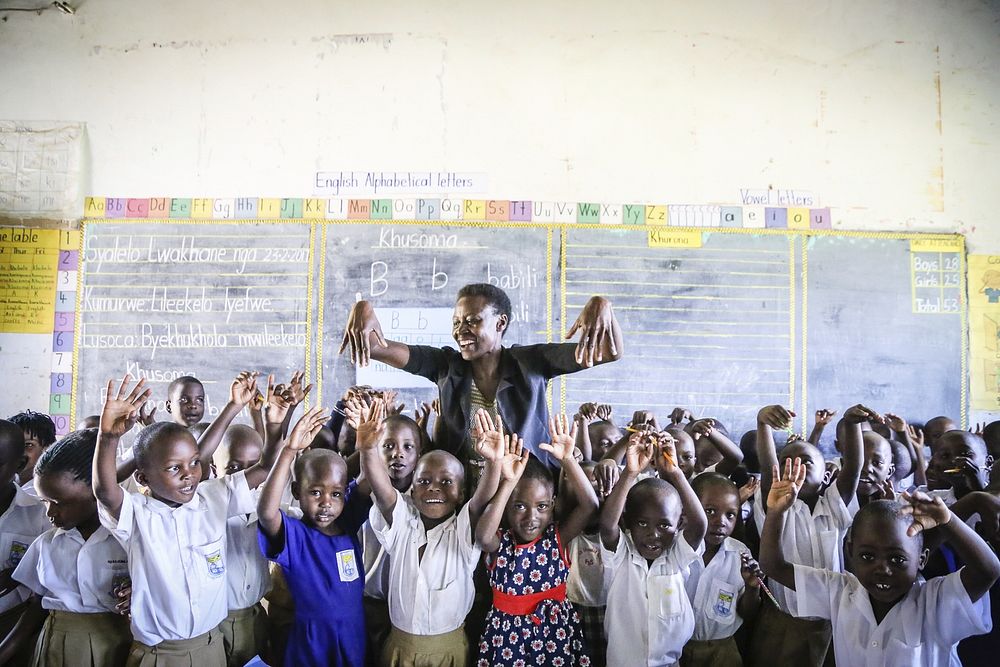
Uganda’s Ministry of Health has enhanced awareness of public health threats like HIV/AIDS by incorporating content into primary and secondary school education. This policy brief advocates for doing the same with content on combating AMR. MSH co-authors include JP Waswa, Reuben Kiggundu, Mohan P. Joshi, Hassan Kasujja, Marion Murungi, Esther Were, Dan Schwarz, and Niranjan Konduri.
Antimicrobial Use across Six Referral Hospitals in Tanzania: A Point Prevalence Survey
This study assessed the factors influencing AMU in six referral hospitals in Tanzania and sought to identify opportunities for enhancing antimicrobial stewardship programs. The findings offer guidance for the development of hospital-specific antimicrobial stewardship programs. MSH co-authors include Edgar Lusaya and Niranjan Konduri.
![[A woman and child visit an accredited dispenser in Tanzania.] {Photo credit: MSH staff}](https://msh.org/wp-content/uploads/2015/06/tanzania_msh_0127_web.jpg)
![[Vincent Nanai conducts routine inventory in the Bariadi District pharmacy store.] {Photo: Michael Bajile/MSH-Tanzania}](https://msh.org/wp-content/uploads/2015/05/tanzania_nanai2_web715.jpg)
Identifying and Addressing Challenges to Antimicrobial Use Surveillance in the Human Health Sector in Low- and Middle-Income Countries: Experiences and Lessons Learned from Tanzania and Uganda
This study explores the challenges in AMU surveillance in Tanzania and Uganda and MTaPS’ efforts enhance skills and establish guidelines for improved AMU surveillance in the region. MSH co-authors include Reuben Kiggundu, Edgar Lusaya, JP Waswa, Dinah Tjipura, Kate Kikule, Cecilia Muiva, Mohan P. Joshi, and Niranjan Konduri.
Antimicrobial Consumption Surveillance in Uganda: Results from an Analysis of National Import Data for the Human Health Sector, 2018–2021
Monitoring antimicrobial consumption is essential for crafting effective antimicrobial stewardship interventions. This study aimed to assess the nationwide use of all antimicrobials in Uganda and identify the requirements for implementing antimicrobial stewardship interventions. MSH co-authors include Marion Murungi, Reuben Kiggundu, JP Waswa, Hassan Kasujja, Ddembe Kaweesi, Mohan P. Joshi, and Niranjan Konduri.


Point Prevalence Survey of Antibiotic Use Across 13 Hospitals in Uganda
This study examines antibiotic use in 13 Ugandan hospitals and highlights areas for enhancing antimicrobial stewardship. MSH co-authors include Reuben Kiggundu, JP Waswa, Marion Murungi, Mohan P. Joshi, and Niranjan Konduri.
Strengthening Multisectoral Coordination on Antimicrobial Resistance: A Landscape Analysis of Efforts in 11 Countries
This article details the challenges and lessons learned by MTaPS in strengthening multisectoral coordination on AMR in 11 countries. Learn how MTaPS worked with host governments to bolster leadership and governance to improve and coordinate AMR activities across sectors. MSH co-authors include Mohan P. Joshi, Tamara Hafner, Antoine Ndiaye, Reuben Kiggundu, Ndinda Kusu, Safoura Berthé, Edgar Lusaya, Alphonse Acho, and Robert Tuala Tuala.
